Diabetic Ulcers
Diabetic ulcers are among the most serious complications of diabetes mellitus, which affects about 15% of diabetic patients in their lifetime. These chronic wounds are difficult to treat and may result in serious consequences if not managed appropriately. This article will discuss the formation, risk factors, and treatment options for diabetic ulcers, with particular emphasis on advanced wound care techniques.
How Do Diabetic Ulcers Form?
Diabetic ulcers are formed by the interplay of many pathophysiological mechanisms. The central role of ulcer formation is taken by peripheral neuropathy, which profoundly alters the sensation of the extremities.
Peripheral Neuropathy: A Central Factor in Ulcer Formation
The reduced sensation creates a dangerous situation in which patients become less aware of pressure points and minor injuries that could lead to the development of a wound. The effects of neuropathy are not limited to mere sensory changes but include the autonomic nervous system: dysfunction of sweat glands and dry skin prone to cracking. Additionally, motor neuropathy leads to muscle imbalances that cause deformities in the foot, creating a set for abnormal pressure points with the potential development of ulcers.
The Role of Vascular Insufficiency in Wound Development
Vascular insufficiency has also been considered a major factor that can cause ulcers. Poor circulation in the extremities, as is notably observed in diabetic patients, grossly diminishes normal healing mechanisms. This effect can be seen at both micro levels of blood vessels as a result of microangiopathy and at larger vessels through atherosclerosis, making it an integrated circulatory problem that makes healing from wounds particularly hard to achieve.
Mechanical Stress and Foot Deformities: Hidden Dangers
The mechanical stress factor cannot be ignored in the process of ulcer formation. Activities that are normally harmless become potentially dangerous in the presence of diabetic complications. Foot deformities create abnormal pressure points, while defective pressure distribution during walking may result in repeated trauma to a specific area, thus contributing to the development of an ulcer.
Key Risk Factors for Diabetic Ulcers
Diabetic ulcers develop from a complex interplay of unmodifiable and modifiable risk factors.
Unmodifiable Risk Factors: Age, Duration of Diabetes, and Genetics
The most important among the unmodifiable factors is the duration of diabetes; patients with a history of more than ten years of diabetes are at significantly higher risks. A past medical history of ulcers or amputation is the strongest predictor of future ulcer occurrence, but advanced age and male gender are also risk factors for developing ulcers. Genetic predisposition to neuropathy can compound all these risks, leading to a complex baseline of factors which healthcare providers must consider in the assessment of patients.
Modifiable Risks: Glycemic Control, Smoking, and Obesity
The modifiable risk factors offer opportunities for intervention and reduction of risk. Poor glycemic control, especially when HbA1c level is >7.0%, significantly increases the risk of ulcers and worsens healing potential. History of smoking adds more vascular complications that might worsen the underlying circulatory problems. Obesity further increases the pressure on the feet.
Foot Care and Hygiene: Everyday Practices That Matter
The daily decisions about foot hygiene and the selection of proper footwear are important preventive measures. Uncontrolled hypertension and a lack of joint mobility also add to the risk profile.
Traditional Approaches to Diabetic Ulcer Care
Diabetic ulcer treatment is performed in a systematic manner, starting with comprehensive wound assessment.
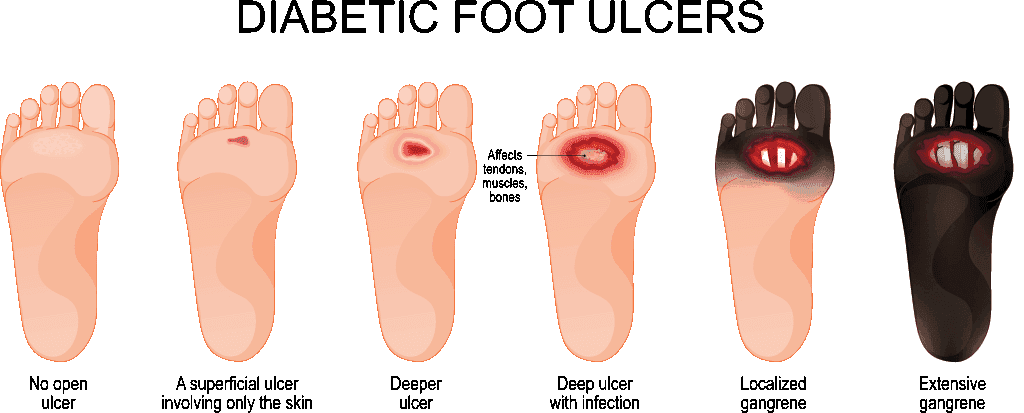
Comprehensive Wound Assessment: The First Step in Treatment
Several factors that clinicians need to assess include the size and depth of the wound, type of tissue, any signs of infection, and vascular status of the affected part of the body. The initial assessment will guide the appropriate treatment strategy.
Offloading Techniques to Relieve Pressure
Offloading is a critical part of any ulcer treatment. It may involve anything from total contact casting to distribute the pressure to the removable cast walker that provides flexibility while offering protection for walking. The correct usage of therapeutic footwear aids greatly both in the course of the treatment and prevention, though several bed rest periods are often necessary as a patient advances through the stages of treatment and rehabilitation.
Wound Bed Preparation: Debridement and Moisture Management
Wound bed preparation forms the foundation of effective treatment. This involves regular debridement to remove necrotic tissue and maintain a healthy wound environment. Maintaining appropriate moisture levels proves crucial, as both excessive dryness and moisture can impede healing. Infection control measures must be implemented consistently, while protecting the periwound skin helps prevent wound expansion.
Choosing the Right Dressings for Optimal Healing
The basic care for a wound includes regular cleaning with appropriate solutions, such as sterile saline or pH-balanced wound cleaners. Selection of dressings should be based on the specific characteristics of the wound, including exudate levels and presence of infection. Hydrocolloid dressings are effective in lightly to moderately exudating wounds, while heavily exudating wounds are better managed with foam dressings.
Advanced Wound Care for Treatment Resistant Diabetic Ulcers
When conventional therapies are not enough, advanced therapies come into play.
The Role of Amniotic Membrane Grafts in Healing Chronic Wounds
Amniotic membrane grafts have gained great importance in the management of treatment resistant diabetic ulcers. These grafts provide necessary growth factors to stimulate tissue regeneration, along with anti-inflammatory cytokines, which help in managing the inflammation of the wound. The natural scaffold structure supports new tissue growth, while angiogenesis-promoting factors help develop new blood vessels crucial for healing.
How Amniotic Grafts Promote Tissue Regeneration and Healing
Amniotic grafts are powerful tools for promoting tissue regeneration and healing in chronic wounds like diabetic ulcers. They contain a rich array of biological components, including growth factors such as VEGF, FGF, and EGF, which stimulate cellular proliferation, differentiation, and angiogenesis. These grafts also provide anti-inflammatory cytokines that reduce inflammation, a common barrier to healing in chronic wounds, while structural proteins like collagen and the extracellular matrix (ECM) create a natural scaffold for tissue remodeling and regeneration. These elements collectively enhance the wound’s ability to repair and rebuild itself efficiently.
There are several types of amniotic products available, each offering unique advantages depending on the wound’s characteristics. Dehydrated human amnion/chorion membranes (dHACM) are easy to store and apply, making them ideal for minimally exudative wounds, while cryopreserved amniotic membranes retain higher biological activity for complex wounds due to minimal processing. Amniotic fluid-derived products, often in liquid form, can be used independently or as adjuncts to other therapies, providing flexibility in treating a variety of wound types.
Amniotic grafts support healing by activating repair mechanisms, enhancing vascularization, and protecting against infection through their antimicrobial properties. They help maintain an optimal wound environment by balancing moisture levels, preventing excess dryness or accumulation. These advanced therapies integrate seamlessly with native tissues, offering clinicians an effective option for managing challenging wounds and improving patient outcomes through a tailored, biologically enhanced approach.
Best Practices for Applying Amniotic Grafts
The application process starts with appropriate preparation of the wound bed, meticulous sizing, and secure fixation of the graft. Monitoring the graft and using appropriate secondary dressings are critical to success.
Post-Graft Care and Long-Term Prevention
Monitoring and Follow-Up for Successful Healing
Successful results with amniotic grafts depend on good post-procedure care. Regular assessments are essential to review graft incorporation and document changes in wound size and characteristics.
Preventing Ulcer Recurrence Through Vigilant Foot Care
Preventing recurrence starts with regular and active foot care. The basis of all these is regular self-examinations, which help patients identify problems before they reach an advanced stage of seriousness. Patients should inspect their feet daily for any redness, swelling, blisters, cuts, or changes in skin texture. A mirror can be used to view the soles and areas between the toes. The early detection of abnormalities allows for early medical treatment that prevents minor issues from becoming chronic wounds.
The Importance of Lifestyle Modifications for Long-Term Success
Lifestyle changes such as smoking cessation, weight management, proper nutrition, and regular exercise significantly reduce the risk of future ulcers and improve overall health.
Conclusion: A Holistic Approach to Managing Diabetic Ulcers
Diabetic ulcers are a major challenge in diabetes management, requiring a holistic understanding of their etiology, risk factors, and treatment options. By combining traditional approaches with advanced therapies like amniotic grafts, healthcare providers can improve patient outcomes. Educating patients and encouraging preventive measures remain key to managing and preventing these complications effectively.
Medical and Insurance Codes
Diabetic ulcers are a significant complication of diabetes mellitus, requiring precise coding for accurate diagnosis and reimbursement. Below is a chart detailing relevant ICD-10-CM diagnosis codes and associated CPT codes for treatment procedures related to diabetic ulcers:
ICD-10-CM Diagnosis Codes:
| ICD-10-CM Code | Description |
|---|---|
| E08.621 | Diabetes mellitus due to underlying condition with foot ulcer |
| E09.621 | Drug or chemical induced diabetes mellitus with foot ulcer |
| E10.621 | Type 1 diabetes mellitus with foot ulcer |
| E11.621 | Type 2 diabetes mellitus with foot ulcer |
| E13.621 | Other specified diabetes mellitus with foot ulcer |
| L97.4- | Non-pressure chronic ulcer of heel and midfoot (requires additional specificity) |
| L97.5- | Non-pressure chronic ulcer of other part of foot (requires additional specificity) |
Note: Codes L97.4- and L97.5- require additional digits to specify laterality (right, left, unspecified) and severity (e.g., limited to breakdown of skin, with fat layer exposed, with necrosis of muscle or bone). For example, L97.511 denotes a non-pressure chronic ulcer of other part of right foot limited to breakdown of skin.
Common CPT Codes for Treatment Procedures:
| CPT Code | Description |
|---|---|
| 97597 | Debridement (e.g., high-pressure waterjet, sharp selective debridement with scissors, scalpel and forceps), open wound, (e.g., fibrin, devitalized epidermis and/or dermis, exudate, debris, biofilm), including topical application(s), wound assessment, and instruction(s) for ongoing care, per session; total wound(s) surface area; first 20 square centimeters or less |
| 97598 | Each additional 20 square centimeters, or part thereof (List separately in addition to code for primary procedure) |
| 11042 | Debridement, subcutaneous tissue (includes epidermis and dermis, if performed); first 20 square centimeters or less |
| 11045 | Each additional 20 square centimeters, or part thereof (List separately in addition to code for primary procedure) |
| 15271 | Application of skin substitute graft to trunk, arms, legs, total wound surface area up to 100 square centimeters; first 25 square centimeters or less |
| 15272 | Each additional 25 square centimeters, or part thereof (List separately in addition to code for primary procedure) |
Note: The selection of CPT codes depends on the specific procedures performed, wound size, and location. Accurate documentation is essential to support the codes billed.
For comprehensive coding, it’s crucial to document the type of diabetes, ulcer location, severity, and any underlying conditions. Always refer to the latest ICD-10-CM and CPT code manuals or official coding guidelines, as codes and billing requirements may change over time.
Diabetic Ulcers
Open sores commonly on the feet, caused by poor blood flow and nerve damage from diabetes. These ulcers can lead to severe infections if untreated.
Chronic Skin Ulcers
Persistent open sores that fail to heal within 4–6 weeks, often caused by poor circulation, pressure, or underlying conditions like diabetes.
Pressure Ulcers
Skin and tissue damage caused by prolonged pressure, typically on bony areas like the hips, heels, or back, common in immobile patients.
Post-Surgical Wounds
Incisions made during surgery that require proper care to prevent infection and promote healing, varying in size and depth.
Venous Stasis Ulcers
Shallow wounds on the lower legs caused by poor blood return to the heart, often accompanied by swelling and discoloration.
Burn Wounds
Skin injuries caused by heat, chemicals, or electricity, ranging in severity from mild redness to deep tissue damage.